What is cognitive behavioral therapy?
Cognitive behavioral therapy (CBT) teaches people to challenge negative thought patterns and turn less often to unhelpful behaviors. These strategies can improve your mood and the way you respond to challenging situations: a flat tire, looming deadlines, family life ups and downs.
Yet there’s much more depth and nuance to this well-researched form of psychotherapy. It has proven effective for treating anxiety, depression, and other mental health conditions. Tailored versions of CBT can also help people cope with insomnia, chronic pain, and other nonpsychiatric conditions. And it can help in managing difficult life experiences, such as divorce or relationship problems.
What are the key components of CBT?
One important aspect of CBT relates to perspective, says psychologist Jennifer Burbridge, assistant director of the Cognitive Behavioral Therapy Program at Harvard-affiliated Massachusetts General Hospital.
“Therapists who practice CBT don’t see the problems or symptoms people describe as having one single cause, but rather as a combination of underlying causes,” she says. These include
- biological or genetic factors
- psychological issues (your thoughts, physical sensations, and behaviors)
- social factors (your environment and relationships).
Each of these factors contributes to — and helps maintain — the troublesome issues that might prompt you to seek therapy, she explains.
How does CBT describe our emotions?
Our emotions have three components: thoughts, physical sensations, and behaviors.
“Thoughts are what we say to ourselves, or 'self-talk,'” says Burbridge. Physical sensations are what we observe in our bodies when we experience an emotional situation: for example, when your heart rate rises in stressful circumstances. Behaviors are simply the things you do — or do not do. For instance, anxiety might prevent you from attending a social event.
All three components are interrelated and influence one another. That’s why CBT helps people to develop skills in each of them. “Think of it as a wellness class for your emotional health,” says Burbridge.
How long does CBT last?
CBT is a goal-oriented, short-term therapy. Typically it involves weekly, 50-minute sessions over 12 to 16 weeks. Intensive CBT may condense this schedule into sessions every weekday over one to three weeks.
Is CBT collaborative?
“When I first meet with someone, I’ll listen to what’s going on with them and start thinking about different strategies they might try,” Burbridge says. But CBT is a collaborative process that involves homework on the patient’s part.
What might that mean for you? Often, a first assignment involves self-monitoring, noting whether there are certain things, events, or times of day that trigger your symptoms. Future sessions focus on fine-tuning approaches to elicit helpful, adaptive self-talk, and problem-solving any obstacles that might prevent progress.
Certain thinking patterns are often associated with anxiety or depression, says Burbridge. Therapists help people recognize these patterns and then work with patients to find broader, more flexible ways to cope with difficult situations.
“We’re cognitive creatures with big frontal lobes that help us analyze situations and solve problems. That’s useful in some situations. But at other times, when you’re trying to manage your emotions, it may be better to pause and acknowledge and accept your discomfort,” says Burbridge.
Which CBT tools and strategies can help?
That particular skill — paying attention in the present moment without judgement, or mindfulness — is a common CBT tool. Another strategy that’s helpful for anxiety, known as exposure or desensitization, involves facing your fears directly.
“People avoid things that make them nervous or scared, which reinforces the fear,” says Burbridge. With small steps, you gradually expose yourself to the scary situation. Each step provides learning opportunities — for example, maybe you realize that the situation wasn’t as scary as you though it would be.
By trying new things instead of avoiding them, you begin to change your thought patterns. These more adaptive thinking patterns then make it more likely you will try new or challenging experiences in the future, thereby increasing your self-confidence.
How does CBT work?
Brain imaging research suggests conditions like depression or anxiety change patterns of activity in certain parts of the brain. One way CBT may help address this is by modifying nerve pathways involved in fear responses, or by establishing new connections between key parts of the brain.
A 2022 review focused on 13 brain imaging studies of people treated with CBT. The analysis suggested CBT may alter activity in the prefrontal cortex (often called the “personality center”) and the precuneus (which is involved in memory, integrating perceptions of the environment, mental imagery, and pain response).
Who might benefit from CBT?
CBT is appropriate for people of all different ages. This can range from children as young as 3 years — in tandem with parents or caregivers — to octogenarians. In addition to treating anxiety and depression, CBT is also effective for
- eating disorders
- substance abuse
- personality disorders
- attention deficit hyperactivity disorder (ADHD)
- obsessive compulsive disorder (OCD).
Additional evidence shows CBT may help people with different health issues, including irritable bowel syndrome, chronic fatigue syndrome, fibromyalgia, insomnia, migraines, and other chronic pain conditions. The therapy may also benefit people with cancer, epilepsy, HIV, diabetes, and heart disease.
“Many medical conditions can limit your activities. CBT can help you adjust to your diagnosis, cope with the new challenges, and still live a meaningful life, despite the limitations,” says Burbridge.
About the Author

Julie Corliss, Executive Editor, Harvard Heart Letter
Julie Corliss is the executive editor of the Harvard Heart Letter. Before working at Harvard, she was a medical writer and editor at HealthNews, a consumer newsletter affiliated with The New England Journal of Medicine. She … See Full Bio View all posts by Julie Corliss
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD
Salmonella is sneaky: Watch out
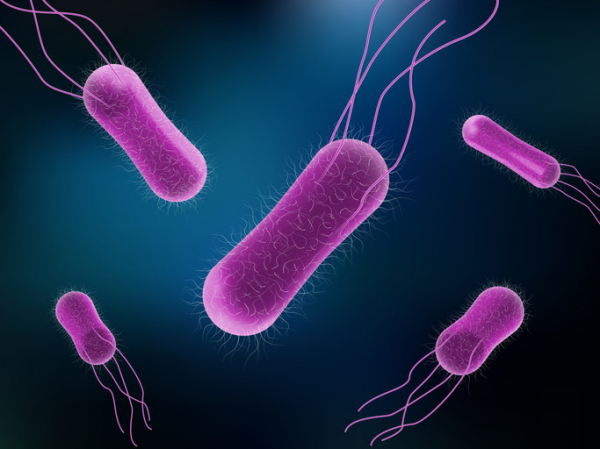
Pop quiz: what is Salmonella? If you’ve ever had a run-in with this bacteria, you know it can cause a food-borne illness called salmonellosis, a form of food poisoning. But you may not know that Salmonella bacteria sicken an estimated 1.35 million people and hospitalize 26,500 every year in the United States. What’s more, it kills more total people than any other type of food poisoning.
And Salmonella bacteria can be sneaky — not only by triggering unusual complications, but infecting people in startling ways, says Dr. Elizabeth Hohmann, an infectious disease specialist at Massachusetts General Hospital. One patient she treated showed up with an abdominal aortic aneurysm — a dangerous bulge in the lower section of the body’s largest artery — that looked infected. Testing revealed a culprit some would find surprising: Salmonella.
“It’s just an interesting organism and it can be kind of scary,” she says.
How do people get infected by Salmonella?
Many of the foods Salmonella bacteria lurk in are raw or undercooked. Breaded raw chicken products like nuggets and chicken Kiev are one way it may reach your table. But a variety of foods have been implicated — including organic basil, cantaloupes, ground beef, nut butters, raw cookie dough, eggs, raw or unpasteurized milk, and flour.
Even small pets such as turtles and frogs, along with dog food, have contributed to Salmonella outbreaks in recent years.
You can also become infected by handling contaminated food and spreading the bacteria from your hands to your mouth. Additionally, you can spread it to others on your hands or even on your clothes without becoming sick yourself.
“It’s a bug that’s carried in stool and animal feces and is also present in the environment,” Dr. Hohmann says. “So it can set up shop in lots of different inanimate objects, soils, and machinery, especially in moist environments.”
What symptoms can Salmonella cause?
Most of the time, Salmonella infection leads to gastroenteritis, usually causing just an upset stomach, abdominal cramps, and diarrhea. These symptoms can start as soon as six hours after ingesting the bacteria. Typically, symptoms resolve on their own within two to three days.
Some people have such mild symptoms they’re barely noticeable. “The classic case might be a college student who eats a burrito from a sketchy place, gets sick for a couple of days, gets better, and doesn’t think anything of it,” says Dr. Hohmann.
Sometimes symptoms are more serious, such as severe abdominal cramping and bloody diarrhea, or unexplained high fever and marked fatigue. These symptoms require a call to your doctor.
How is salmonellosis treated?
Most people will get better on their own without any medicines. Replacing lost fluids by sipping water or electrolyte drinks to avoid dehydration will help.
Call a doctor if you have
- diarrhea and a fever higher than 102° F
- diarrhea that doesn’t improve after three days
- bloody stools
- vomiting so severe it prevents you from keeping liquids down.
Treating the infection with medicine comes with an annoying paradox, Dr. Hohmann says. If doctors decide to prescribe antibiotics, the person taking the medicine may shed the organism for longer than if they were never treated. “Then that person may have the opportunity — either through poor personal hygiene, sex, or working as a food worker — to spread it to others,” she explains. “It’s challenging.”
What complications can Salmonella lead to?
Some people get sicker with salmonellosis than others, with seemingly no rhyme or reason. But certain folks are especially vulnerable to serious infection, including:
- adults 65 and older
- pregnant women
- children under 5
- people whose immune systems are weakened by diseases (such as cancer) or treatments (such as immunosuppressing drugs).
A small percentage of those infected can have Salmonella in their blood, which can spread the infection to other parts of the body such as the urinary tract, bones, joints, or central nervous system (brain and spinal fluid).
And, like Dr. Hohmann’s patient with the abdominal aortic aneurysm, on rare occasions Salmonella can lead to unusual blood vessel complications in people who already have atherosclerosis, blockage of the arteries caused by plaque buildup.
“It’s not that common,” she says. “Many physicians are aware of it, so they take special care if Salmonella is found in a person with vascular disease.”
What steps can you take to avoid Salmonella?
While new USDA rules that take effect in 2025 may help fuel recalls of certain foods, we all can take steps to avoid the food poisoning, illness, and hospitalizations that Salmonella exposure can cause.
Dr. Hohmann and the CDC suggest these strategies:
- Using hot water and soap, wash cutting boards or plates on which you cut into raw foods — including vegetables and fruit — before using those surfaces for other purposes. If possible, use separate cutting boards for produce, meat, and fish.
- Refrigerate or freeze foods that are perishable, prepared, or left over within two hours to thwart salmonella growth.
- Always wash hands well with soap and water before preparing food and after contact with animals, using the toilet, or changing diapers.
- If you have a sick pet, take extra care handling its feces and wash your hands thoroughly afterward.
Take additional steps to help more vulnerable people stay healthy:
- Don’t let young children touch high-risk animals, such as turtles, frogs, chickens, or ducks. “And if you’re taking young children to a petting zoo, they should not be petting animals unless you can disinfect their hands immediately afterward,” she says.
- Older adults and those with compromised immune systems should take extra care to wash and cook foods thoroughly.
- People who have had a transplant (such as a kidney transplant) should not keep reptiles or amphibians as pets.
“You hate to make people paranoid, so that we’re washing our lettuce leaves with soap, but it’s worth thinking about these things, particularly if you have people in your household who are susceptible — which is an increasing number of people,” Dr. Hohmann says.
About the Author

Maureen Salamon, Executive Editor, Harvard Women's Health Watch
Maureen Salamon is executive editor of Harvard Women’s Health Watch. She began her career as a newspaper reporter and later covered health and medicine for a wide variety of websites, magazines, and hospitals. Her work has … See Full Bio View all posts by Maureen Salamon
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

Swimming lessons save lives: What parents should know

Before going any further, here’s the main thing parents should know about swimming lessons: all children should have them.
Every year, over 4,500 people die from drowning in the United States — and, in fact, drowning is the leading cause of death for children ages 1 to 4. Swimming lessons can’t prevent all of those deaths, but they can prevent a lot of them. A child doesn’t need to be able to swim butterfly or do flip turns, but the ability to get back to the surface, float, tread water, and swim to where they can stand or grab onto something can save a life.
10 things parents should know about swimming lessons
As you think about swimming lessons, it’s important to know:
1. Children don’t really have the cognitive skills to learn to swim until they are around 4 years old. They need to be able to listen, follow directions, and retain what they’ve learned, and that’s usually around 4 years old, with some kids being ready a little earlier.
2. That said, swim lessons between 1 and 4 years old can be useful. Not only are some kids simply ready earlier, younger children can learn some skills that can be useful if they fall into the water, like getting back to the side of a pool.
3. The pool or beach where children learn must be safe. This sounds obvious, but safety isn’t something you can assume; you need to check it out for yourself. The area should be clean and well maintained. There should be lifeguards that aren’t involved in teaching (since teachers can’t be looking at everyone at all times). There should be something that marks off areas of deeper water, and something to prevent children from getting into those deeper areas. There should be lifesaving and first aid equipment handy, and posted safety rules.
4. The teachers should be trained. Again, this sounds obvious — but it’s not always the case. Parents should ask about how teachers are trained and evaluated, and whether it’s under the guidelines of an agency such as the Red Cross or the YMCA.
5. The ratio of kids to teachers should be appropriate. Preferably, it should be as low as possible, especially for young children and new swimmers. In those cases, the teacher should be able to have all children within arm’s reach and be able to watch the whole group. As children gain skills the group can get a bit bigger, but there should never be more than the teacher can safely supervise.
6. There should be a curriculum and a progression — and children should be placed based on their ability. In general, swim lessons progress from getting used to the water all the way to becoming proficient at different strokes. There should be a clear way that children are assessed, and a clear plan for moving them ahead in their skills.
7. Parents should be able to watch for at least some portion. You should be able to see for yourself what is going on in the class. It’s not always useful or helpful for parents to be right there the whole time, as it can be distracting for children, but you should be able to watch at least the beginning and end of a lesson. Many pools have an observation window or deck.
8. Flotation devices should be used thoughtfully. There is a lot of debate about the use of “bubbles” or other flotation devices to help children learn to swim. They can be very helpful with keeping children safe at the beginning, and helping them learn proper positioning and stroke mechanics instead of swimming frantically to stay afloat, but if they are used, the lessons should be designed to gradually decrease any reliance on them.
9. Being scared of the water isn’t a reason not to take, or to quit, swimming lessons. It’s common and normal to be afraid of the water, and some children are more afraid than others. While you don’t want to force a child to do something they are terrified of doing, giving up isn’t a good idea either. Start more gradually, with lots of positive reinforcement. The swim teacher should be willing to help.
10. Just because a child can swim doesn’t mean he can’t drown. Children can get tired, hurt, trapped, snagged, or disoriented. Even strong swimmers can get into trouble. While swimming lessons help save lives, children should always, always be supervised around water, and should wear life jackets for boating and other water sports.
The Centers for Disease Control and Prevention website has helpful information on preventing drowning. The American Red Cross offers an online water safety course for caregivers and parents and water safety videos for children. Many public pools and organizations like Boys & Girls Clubs and the YMCA offer swimming classes for all ages.
About the Author

Claire McCarthy, MD, Senior Faculty Editor, Harvard Health Publishing
Claire McCarthy, MD, is a primary care pediatrician at Boston Children’s Hospital, and an assistant professor of pediatrics at Harvard Medical School. In addition to being a senior faculty editor for Harvard Health Publishing, Dr. McCarthy … See Full Bio View all posts by Claire McCarthy, MD
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

Ultra-processed foods? Just say no

Americans love their ultra-processed foods, whether they come as cereal (like Cap’n Crunch, a favorite of mine as a kid), snack foods (like Cheetos), entr’es (like hot dogs), or desserts (like Twinkies). Sure, loading your plate with vegetables, fruits, fish, healthful oils, and grains in a Mediterranean-style diet boosts heart and brain health. But if you also eat some ultra-processed foods, is that bad for your brain health?
What to know about this new study
A new study appears to deliver resounding yes: eating ultra-processed foods is linked to a greater risk of cognitive impairment and strokes.
This well-designed observational study examined data from the REGARDS (REasons for Geographic And Racial Differences in Stroke) project, a longitudinal study of non-Hispanic Black and white Americans ages 45 years and older. Study participants were initially enrolled between 2003 and 2007 and were given a number of questionnaires evaluating health, diet, exercise, body mass index, education, income, alcohol use, mood, and other factors. In addition, tests of memory and language were administered at regular intervals.
To examine the risk of stroke and cognitive impairment, data from 20,243 and 14,175 participants, respectively, were found usable based on the quality of the information from the questionnaires and tests. Approximately one-third of the sample identified as Black and the majority of the remaining two-thirds identified as white.
The results of the study
- According to the authors’ analysis, increasing the intake of ultra-processed foods by just 10% was associated with a significantly greater risk of cognitive impairment and stroke.
- Intake of unprocessed or minimally processed foods was associated with a lower risk of cognitive impairment.
- The effect of ultra-processed foods on stroke risk was greater for individuals who identified as Black compared to individuals who identified as white.
Study participants who reported following a healthy diet (like a Mediterranean, DASH, or MIND diet) and consumed minimal ultra-processed foods appeared to maintain better brain health compared to those who followed similar healthy diets but had more ultra-processed foods.
Why might ultra-processed foods be bad for your brain?
Here are some biologically plausible reasons:
- UPFs are generally composed of processed carbohydrates that are very quickly broken down into simple sugars, equivalent to eating lots of candy. These sugar loads cause spikes of insulin, which can alter normal brain cell function.
- Eating ultra-processed foods is associated with a higher risk of metabolic syndrome and obesity, well-established conditions linked to high blood pressure, abnormal blood lipid levels, and type 2 diabetes.
- There are unhealthy additives in ultra-processed foods to change the texture, color, sweetness, or flavor. These additives disrupt the microbiome in the gut and can lead to gut inflammation that can cause
- the production of microbiome-produced metabolites that can affect brain function (such as short-chain fatty acids and lipopolysaccharides)
- leaky gut, allowing toxins and inflammatory molecules to enter the bloodstream and go to the brain
- altered neurotransmitter function (such as serotonin) that can impact mood and cognition directly
- increased cortisol levels that mimic being under chronic stress, which can directly impact hippocampal and frontal lobe function, affecting memory and executive function performance, respectively
- an increased risk for Alzheimer’s, Parkinson’s, and other neurodegenerative diseases due to inflammatory molecules traveling from the gut to the brain.
- Because ultra-processed foods have poor nutritional value, people will often be hungry shortly after eating them, leading to overeating and its consequences.
The take-home message
Avoid processed foods, which can include chips and other snack foods, industrial breads and pastries, packaged sweets and candy, sugar-sweetened and diet sodas, instant noodles and soups, ready-to-eat meals and frozen dinners, and processed meats such as hot dogs and bologna. Eat unprocessed or minimally processed foods, which — when combined with a healthy Mediterranean menu of foods — include fish, olive oil, avocados, whole fruits and vegetables, nuts and beans, and whole grains.
About the Author
Andrew E. Budson, MD, Contributor; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Andrew E. Budson is chief of cognitive & behavioral neurology at the Veterans Affairs Boston Healthcare System, lecturer in neurology at Harvard Medical School, and chair of the Science of Learning Innovation Group at the … See Full Bio View all posts by Andrew E. Budson, MD

Power your paddle sports with three great exercises

On the Gulf Coast of Florida where I live, the telltale sign of summer is not an influx of beachcombers, afternoon storms that arrive exactly at 2 p.m., or the first hurricane warning, but the appearance of hundreds of paddleboarders dotting the inlet waters.
From afar, paddleboarding looks almost spiritual — people standing on nearly invisible boards and gliding across the surface as if walking on water.
But this popular water sport offers a serious workout, just as kayaking and canoeing do. While floating along and casually dipping a paddle in the water may look effortless, much goes on beneath the surface, so to speak.
As warm weather beckons and paddle season arrives, it pays to get key muscles in shape before heading out on the water.
Tuning up muscles: Focus on core, back, arms, and shoulders
“Paddling a kayak, canoe, or paddleboard relies on muscles that we likely haven’t used much during winter,” says Kathleen Salas, a physical therapist with Spaulding Adaptive Sports Centers at Harvard-affiliated Spaulding Rehabilitation Network. “Even if you regularly weight train, the continuous and repetitive motions involved in paddling require endurance and control of specific muscles that need to be properly stretched and strengthened.”
While paddling can be a whole-body effort (even your legs contribute), three areas do the most work and thus need the most conditioning: the core, back, and arms and shoulders.
- Core. Your core comprises several muscles, but the main ones for paddling include the rectus abdominis (that famed “six-pack”) and the obliques, located on the side and front of your abdomen. The core acts as the epicenter around which every movement revolves — from twisting to bending to stabilizing your trunk to generate power.
- Back: Paddling engages most of the back muscles, but the ones that carry the most load are the latissimus dorsi muscles, also known as the lats, and the erector spinae. The lats are the large V-shaped muscles that connect your arms to your vertebral column. They help protect and stabilize your spine while providing shoulder and back strength. The erector spinae, a group of muscles that runs the length of the spine on the left and right, helps with rotation.
- Arms and shoulders: Every paddle stroke engages the muscles in your arms (biceps) and the top of your shoulder (deltoids).
Many exercises specifically target these muscles, but here are three that can work multiple paddling muscles in one move. Add them to your workouts to help you get ready for paddling season. If you haven’t done these exercises before, try the first two without weights until you can do the movement smoothly and with good form.
Three great exercises to prep for paddling
Wood chop


Muscles worked: Deltoids, obliques, rectus abdominis, erector spinae
Reps: 8–12 on each side
Sets: 1–3
Rest: 30–90 seconds between sets
Starting position: Stand with your feet about shoulder-width apart and hold a dumbbell with both hands. Hinge forward at your hips and bend your knees to sit back into a slight squat. Rotate your torso to the right and extend your arms to hold the dumbbell on the outside of your right knee.
Movement: Straighten your legs to stand up as you rotate your torso to the left and raise the weight diagonally across your body and up to the left, above your shoulder, while keeping your arms extended. In a chopping motion, slowly bring the dumbbell down and across your body toward the outside of your right knee. This is one rep. Finish all reps, then repeat on the other side. This completes one set.
Tips and techniques:
- Keep your spine neutral and your shoulders down and back
- Reach only as far as is comfortable.
- Keep your knees no farther forward than your toes when you squat.
Make it easier: Do the exercise without a dumbbell.
Make it harder: Use a heavier dumbbell.
Bent-over row


Muscles worked: Latissimus dorsi, deltoids, biceps
Reps: 8–12
Sets: 1–3
Rest: 30–90 seconds between sets
Starting position: Stand with a weight in your left hand and a bench or sturdy chair on your right side. Place your right hand and knee on the bench or chair seat. Let your left arm hang directly under your left shoulder, fully extended toward the floor. Your spine should be neutral, and your shoulders and hips squared.
Movement: Squeeze your shoulder blades together, then bend your elbow to slowly lift the weight toward your ribs. Return to the starting position. Finish all reps, then repeat with the opposite arm. This completes one set.
Tips and techniques:
- Keep your shoulders squared throughout.
- Keep your elbow close to your side as you lift the weight.
- Keep your head in line with your spine.
Make it easier: Use a lighter weight.
Make it harder: Use a heavier weight.
Superman


Muscles worked: Deltoids, latissimus dorsi, erector spinae
Reps: 8–12
Sets: 1–3
Rest: 30–90 seconds between sets
Starting position: Lie face down on the floor with your arms extended, palms down, and legs extended.
Movement: Simultaneously lift your arms, head, chest, and legs off the floor as high as is comfortable. Hold. Return to the starting position.
Tips and techniques:
- Tighten your buttocks before lifting.
- Don’t look up.
- Keep your shoulders down, away from your ears.
Make it easier: Lift your right arm and left leg while keeping the opposite arm and leg on the floor. Switch sides with each rep.
Make it harder: Hold in the “up” position for three to five seconds before lowering.
About the Author

Matthew Solan, Executive Editor, Harvard Men's Health Watch
Matthew Solan is the executive editor of Harvard Men’s Health Watch. He previously served as executive editor for UCLA Health’s Healthy Years and as a contributor to Duke Medicine’s Health News and Weill Cornell Medical College’s … See Full Bio View all posts by Matthew Solan
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

Packing your hurricane go bag? Make provisions for your health

When you live in a coastal area, preparing early for potential hurricanes is a must. Storms can develop quickly, leaving little time to figure out where you’ll be safe or which items to pack if you have to evacuate. And health care necessities, such as medications or medical equipment, are often overlooked in the scramble.
“People might bring their diabetes medication but forget their blood sugar monitor, or bring their hearing aids but forget extra batteries for them,” says Dr. Scott Goldberg, medical director of emergency preparedness at Brigham and Women’s Hospital and a longtime member of a FEMA task force that responds to hurricane-damaged areas.
Here’s some insight on what to expect this hurricane season, and how to prioritize health care in your hurricane kit.
What will the 2024 hurricane season look like?
This year’s hurricane predictions underscore the urgency to start preparations now.
Forecasters with the National Oceanic and Atmospheric Administration’s National Weather Service expect above-normal activity for the 2024 hurricane season (which lasts until November 30).
Meteorologists anticipate 17 to 25 storms with winds of 39 mph or higher, including eight to 13 hurricanes — four to seven of which could be major hurricanes with 111 mph winds or higher.
What kinds of plans should you make?
Preparing for the possibility of big storms is a major undertaking. Long before ferocious winds and torrential rains arrive, you must gather hurricane supplies, figure out how to secure your home, and determine where to go if you need to evacuate (especially if you live in a flood zone). Contact the emergency management department at your city or county for shelter information.
If you’ll need help evacuating due to a medical condition, or if you’ll need medical assistance at a shelter, find out if your county or city has a special needs registry like this one in Florida. Signing up will enable first responders to notify you about storms and transport you to a special shelter that has medical staff, hospital cots, and possibly oxygen tanks.
What should you pack?
While a shelter provides a safe place to ride out a storm, including bathrooms, water, and basic meals, it’s up to you to bring everything else. It’s essential to pack medical equipment and sufficient medications and health supplies.
“It’s natural to just grab the prescription medications in your medicine cabinet, but what if it’s only a two-day supply? It might be a while before you can get a refill. We recommend at least a 14-day or 30-day supply of every prescription,” Dr. Goldberg says. “Talk to your doctor about the possibility of getting an extra refill to keep on standby for your go bag.”
Other health-related items you’ll want to pack include:
- medical supplies you use regularly, such as a blood pressure monitor, heart monitor, CPAP machine, wheelchair, or walker
- over-the-counter medicines you use regularly, such as heartburn medicine or pain relievers
- foods for specific dietary needs, such as gluten-free food if you have celiac disease (if you have infants or children, you’ll need to bring foods they can eat)
- healthy, nonperishable snacks such as nuts, nut butters, trail mix, dried fruit, granola bars, protein bars, and whole-grain bread, crackers, or cereals
- hygiene products such as soap, hand sanitizer, toothbrushes and toothpaste, shampoo, deodorant, infant or adult diapers, lip balm, moist towelettes, and toilet paper — because shelters often run out of it.
Remember the basics
In some ways, you can think of shelter living like camping. You’ll need lots of basic supplies to get through it, including:
- a sleeping bag or blanket and pillow for each person in your family
- clean towels and washcloths
- a few extra changes of clothes per person
- a first-aid kit
- flashlights and extra batteries
- chargers for your electronic gadgets
- rechargeable battery packs.
Bring important paperwork
In addition to supplies, bring important documents such as:
- a list of your medications, vitamins, and supplements (include the name, dose, and frequency of each one)
- a list of the names, addresses, and phone numbers of your primary care provider and any specialists who treat you
- a list of your emergency contacts and their phone numbers
- your pharmacy’s phone number and address
- copies of your birth certificate and driver’s license
- copies of home, car, or life insurance policies
- copies of your health insurance cards
- a copy of your advance directive — which includes your living will and health care proxy form.
“Store these documents on a flash drive. Also make photocopies of them, which are easiest for doctors to consult in an emergency setting. Place them in a plastic zip-top bag to keep them dry,” Dr. Goldberg advises.
Prepare right now
Start today. Gather as many go-bag supplies as you can, including the bags. A small suitcase, backpack, or duffel bag for each person in your family will work well.
And try not to put off these important preparations. “Hurricanes are major stressors. You might be worried, sleep deprived, fatigued, and emotional,” Dr. Goldberg says. “All of that will make it hard to think clearly. You’ll do yourself and your family a favor by having discussions now and getting started on your hurricane plan.”
About the Author

Heidi Godman, Executive Editor, Harvard Health Letter
Heidi Godman is the executive editor of the Harvard Health Letter. Before coming to the Health Letter, she was an award-winning television news anchor and medical reporter for 25 years. Heidi was named a journalism fellow … See Full Bio View all posts by Heidi Godman
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

Health care should improve your health, right?

It’s undeniable: modern medicine offers ever-expanding ways to heal and prevent disease. But it’s also true that health care can cause harm. One analysis found that about 6% of health care encounters caused preventable harm, leading to thousands of deaths each year. And it’s not just errors that cause trouble. Highly skilled health care providers can cause harm even when they do everything right.
So, how can you reduce your chances of being harmed? Understanding what you can do to lessen the possibility of harm and what’s beyond your control are good first steps.
Whatever happened to “first do no harm”?
Fortunately, it remains a central tenet of medical care. Yet our health care system is complex and fragmented. Each year new medications are added to an ever-growing list, and people live longer with more chronic medical conditions than happened in the past. So in one sense, the successes of modern medical care may contribute to the high rate of health care–related harm.
These harms are often due to our complicated system of health care rather than one individual’s mistake. Harm due to substandard or negligent care is known as medical malpractice. Both health care providers and health care systems have important roles to play in preventing harm to patients.
Are there harms that cannot be prevented?
An enormous volume of scientific research teaches the best ways to diagnose, treat, and prevent disease. Yet people can react to treatments in completely unpredictable ways.
For example, a common and standard antibiotic treatment (think penicillin) can cause anaphylaxis, a life-threatening allergic reaction. Fortunately this is rare, but unless you or your doctor know to avoid it due to past side effects, there’s always a small chance of a severe reaction.
Often less dramatic — yet also unpreventable — harms are:
- Medication side effects. Every medicine comes with potential side effects, such as nausea, sleepiness, or rash.
- Misdiagnosis. Because no one has perfect diagnostic skills, even the most skillful health care provider can be wrong. This can result in unnecessary or delayed treatment.
- Inaccurate test results. Just as no health care provider is perfect, no test is either. False-positive results (indicating an abnormality when none is present) and false-negative results (normal results when disease is present) are common in medical practice. These results can lead to unnecessary treatment or false reassurance.
Which harms can be prevented?
Preventable harms can be dramatically reduced. They’re often due to mistakes that can be caught and corrected. Frequently, it takes a combination of things to go wrong for harm to occur.
The “Swiss cheese model” is often applied here: imagine you’re a fly trying to travel through several chunks of Swiss cheese. (I know it’s an odd scenario, but stick with me here.) It’s impossible to fly through the cheese unless the holes line up just so.
Frequently in health care, several factors must line up for an error to sneak through — for example, giving a hospitalized patient a medication to which they are allergic. For that to happen, the wrong drug has to get past the prescribing doctor, the computerized ordering system, the hospital pharmacist, the nurse giving the medication, and the patient. That’s a lot of layers, so most often an error like this will be caught.
What can you do to avoid preventable harms?
Where do you fit in? In these three scenarios, here’s what you can do to avoid preventable harms.
The problem: Taking medicines you no longer need or more medicines than necessary.
It might not seem like a big deal to keep taking a medicine if it isn’t causing any problems. But all medicines can cause side effects that you’d do better to avoid if you can safely stop taking it or reduce the dose. Plus, harmful interactions can occur if another medicine is added to your list.
What you can do: Make sure you know why you need to take each of your medicines. Ask the providers who prescribe each medicine if it is still necessary to take it or if the dose can be safely reduced. Reducing a dose may reduce the risk of side effects and the likelihood of a harmful interaction.
The problem: Taking the wrong medicine or the wrong dose.
What you can do: At your doctors’ visits, take notes or bring a friend or family member to help you remember medicine instructions. Ask whether you can record the medication instructions your doctor gives you. Take a photo of the instructions you’re given in case you lose the written version. Double-check details of your medicine list with your pharmacist. And ask questions if you’re unsure about the medicines recommended to you.
The problem: Wrong site surgery.
Despite efforts to make this a “never error,” surgery on the wrong part of the body still happens.
What you can do: Make sure you and your surgeon agree on what part of your body and which side requires surgery. Most surgeons now mark the site with a special pen before surgery and ask you to confirm the site by adding your initials. (The ink doesn’t come off easily with skin cleaners applied prior to surgery).
Some of these tips require time or resources that aren’t available to everyone: you might not be able to bring another person with you to medical visits or have a recording device. But asking questions — and getting answers you understand — should be routine.
Where does malpractice fit in?
When the topic of health care–related harm comes up, malpractice may be the first thing you think about. Yet, the approximately 10,000 malpractice payments made each year in the US likely represent only a small portion of all harm related to health care.
There are several reasons for this, including:
- Even when negligent or substandard care occurs, it doesn’t always cause major or long-lasting harm that leads to a malpractice claim.
- Many people who could file malpractice suits elect not to, or may not even realize that they’ve experienced negligent care. Past studies suggest that less than 5% of people experiencing harm related to medical care file malpractice claims.
- Increasingly, health care providers and health care systems accept responsibility for preventable harm occurring on their watch, and offer compensation rather than waiting for a legal claim to be filed.
The bottom line
It’s an unfortunate reality that some harms due to health care are inevitable. But there are steps you can take to avoid preventable harm and lessen the chances that the person harmed is you.
About the Author
Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. … See Full Bio View all posts by Robert H. Shmerling, MD

Shining light on night blindness

Animals renowned for their outstanding night vision include owls, cats, tarsiers (a tiny primate in Southeast Asia) — and even the dung beetle.
But humans? Not so much.
Over time, many people suffer from night blindness, also known as nyctalopia. This condition makes seeing in dim or dark settings difficult because your eyes cannot adjust to changes in brightness or detect light.
What are the dangers for those experiencing night blindness?
Night blindness is especially problematic and dangerous when driving. Your eyes cannot adjust between darkness and the headlights of oncoming vehicles, other cars may appear out of focus, and your depth perception becomes impaired, which makes it difficult to judge distances.
Night blindness also may affect your sight at home by making it hard for your vision to quickly adjust to a dark room after turning off the lights. “This can cause people to bump into furniture or trip and suffer an injury,” says Dr. Isabel Deakins, an optometrist with Harvard-affiliated Massachusetts Eye and Ear.
What happens in the eye to create night blindness?
The ability to see in low-light conditions involves two structures in the eye: the retina and the iris.
The retina, located in the back of the eye, contains two types of light-detecting cells called cones and rods. The cones handle color vision and fine details while the rods manage vision in dim light.
The iris is the colored part of your eye. It contains muscles that widen or narrow the opening of your pupil to adjust how much light can enter your eyes.
If your irises don’t properly react, the pupils can dilate and let in too much light, which causes light sensitivity and makes it hard to see in bright light. Or your pupils may remain too small and not allow in enough light, making it tough to see in low light.
What causes night blindness?
Night blindness is not a disease but a symptom of other conditions. “It’s like having a bruise on your body. Something else causes it,” says Dr. Deakins.
Several conditions can cause night blindness. For instance, medications, such as antidepressants, antihistamines, and antipsychotics, can affect pupil size and how much light enters the eye.
Eye conditions that can cause night blindness include:
- glaucoma, a disease that damages the eye’s optic nerves and blood vessels
- cataracts, cloudy areas in the lens that distort or block the passage of light through the lens
- dry eye syndrome.
However, one issue that raises the risk of night blindness that you can’t control is age. “Our eyes react more slowly to light changes as we age, and vision naturally declines over time,” says Dr. Deakins. “The number of rods in our eyes diminish, pupils get smaller, and the muscles of the irises weaken.”
What helps if you have night blindness?
If you notice any signs of night blindness, avoid driving and get checked by an eye care specialist like an optometrist or ophthalmologist. An eye exam can determine if your eyeglass prescription needs to be updated.
“Often, a prescription change is enough to reduce glare when driving at night," says Dr. Deakins. “You may even need separate glasses with a stronger eye prescription that you wear only when driving at night.”
Adding an anti-reflective coating to your lens may help to cut down on the glare of the headlights of an oncoming car. However, skip the over-the-counter polarized driving glasses sold at many drug stores. "These may help cut down on glare, but they don't address the causes of night blindness," says Dr. Deakins.
An eye exam also will identify glaucoma or cataracts, which can be treated. Glaucoma treatments include eyedrops, laser treatment, or surgery. Cataracts are corrected with surgery to replace the clouded lens with an artificial one. Your eye care specialist can also help identify dry eye and recommend treatment.
Ask your primary care clinician or a pharmacist if any medications that you take may cause night blindness. If so, it may be possible to adjust the dose or switch to another drug.
Three more ways to make night driving safer
You also can take steps to make night driving safer. For example:
- Wash the lenses of your glasses regularly. And take them to an optician to buff out minor scratches.
- Keep both sides of your front and rear car windshields clean so that you can see as clearly as possible.
- Dim your dashboard lights, which cause glare, and use the night setting on your rearview mirror.
About the Author

Matthew Solan, Executive Editor, Harvard Men's Health Watch
Matthew Solan is the executive editor of Harvard Men’s Health Watch. He previously served as executive editor for UCLA Health’s Healthy Years and as a contributor to Duke Medicine’s Health News and Weill Cornell Medical College’s … See Full Bio View all posts by Matthew Solan
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

Ever read your medical record? Here’s why you should

Do you ever read the notes written by your doctor or health practitioner during a medical visit? If not, you might want to check them out. Usually, these medical notes are full of helpful insights about your health and reminders of recommendations discussed. And there’s medicalese, of course: hard-to-pronounce illnesses, medications, and technical terms.
But you may be surprised to see incorrect information or unexpected language, tone, or even innuendo. Was your past medical history really that “unremarkable”? Did you actually “deny” drinking alcohol? Did the note describe you as “unreliable”?
Here’s how to decipher unfamiliar lingo, understand some surprising descriptions, and flag any errors you find.
What’s in a medical note?
A standard medical note has several sections. These include
- a description of current symptoms
- past medical problems
- a list of medications taken
- family medical history
- social habits such as smoking, drinking alcohol, or drug use
- details of the physical examination
- test results
- a discussion of the big picture, along with recommendations for further evaluation or treatment.
Notes tend to be more complete for a new patient or annual exam. Follow-up notes may not cover all of these points.
What’s potentially confusing about medical notes?
Most medical notes aren’t written using plain language because they aren’t intended primarily for a nonmedical audience. So it’s common to run across:
- Medical jargon: You had an upset stomach and a fever. Doctors may say “dyspepsia” (upset stomach) and “febrile” (fever).
- Complicated disease names: Ever heard of “multicentric reticulohistiocytosis” or “progressive multifocal leukoencephalopathy?” These are just two of thousands of examples.
- Use of common language in uncommon ways: For example, your medical history might be called “unremarkable” and test results called "within normal limits” rather than “normal.”
- Abbreviations: You might see “VSS” and “RRR,” meaning “vital signs stable” with a pulse that has a “regular rate and rhythm.”
If you’re having trouble deciphering a note or understanding your health issues, tests, and recommendations, check in with your doctor’s office for clarifications. The more you understand about your health and your options for care, the better.
What if a medical note is incorrect?
Minor errors in medical notes are not rare: maybe you had your tonsils removed 30 years ago, not 10 years ago. But there can be more important errors: stating that arthritis in your left knee is severe when it’s actually the right knee that’s severe could lead to having x-rays (or even surgery!) on the wrong side. And not properly recording a family history of cancer or heart disease could mean missing out on timely screening tests or preventive treatments.
In an era of ever-increasing time pressure, use of voice recognition software, electronic record templates, drop-down menus, and ability to copy and paste text, it’s easier than ever for health care providers to make (and perpetuate) errors in the medical record.
If you do see an important error that could affect your health, ask your provider to amend it.
What if the language in a medical note seems offensive?
Numerous studies have highlighted the problem of stigmatizing language in medical notes that can leave people feeling judged or offended. Negative attitudes can affect the quality of our health care and willingness to seek care, and can also widen health disparities. One study linked stigmatizing language to higher rates of medical errors. Of note, this study found higher rates of stigmatizing language and medical error among black patients.
Examples include:
- Depersonalization: A note might describe a patient as “a drug abusing addict” rather than a person struggling with drug addiction.
- Insulting or inappropriate descriptors: Notes might contain subjective descriptions that paint the patient in an unflattering light without providing context. For example, the note might say “the patient is unkempt and is drug-seeking” rather than “the patient is experiencing homelessness and has severe, chronic pain.” If a person’s recall of medical events from the past is hazy, they may be called “unreliable.”
- Dismissiveness: A medical note may suggest a symptom is not real or is exaggerated, rather than taking the complaint seriously.
- An untrusting tone: Language such as “she claims she never drinks” or “he denies alcohol use” may suggest mistrust by the physician.
Why might this happen, anyway?
How does such language make its way into medical notes? (To be clear, these possible explanations are not justifications.)
- Tradition and training: Medical trainees, like other learners, tend to follow the lead of their mentors. So if stigmatizing language is used by an instructor, trainees may do the same.
- Time pressure: With medical documentation (as in most everything else), mistakes are more common if you’re rushing.
- Bias: Like everyone else, doctors have biases, including ones they aren’t aware of. How we are taught to think about people — by family, by society — can spill over into every area of life, including work.
- Frustration: Doctors may feel frustrated by patients who don’t follow their recommendations. That frustration can be reflected in their medical notes. For example, a note may say, “As expected, the patient’s blood sugar is high; he is still not checking his blood sugar or following the diet recommended by his nutritionist.”
If the language in a note is confusing or bothersome, ask about it. The Open Notes movement and federal legislation have given most of us much better access to our medical records. This has worthy goals — greater transparency and better communication with people about their medical care — and unintended consequences.
Is changing language in notes that health practitioners once shared mainly with each other a positive consequence? Mostly. Yet some doctors worry that notes will become less specific, accurate, or useful since they may leave out information that might upset a patient.
The bottom line
I encourage you to read your health providers’ notes about your care. If there is a substantial error or something you find confusing or objectionable, ask about it. By the way, a signed medical note cannot usually be revised. However, your doctor can make clarifications or correct mistakes in an addendum at the end of the note.
As more and more patients read their medical notes, it’s likely that health providers will be more conscientious about the language they use. So, wide access to medical notes may improve not only people’s understanding of their health, but also the quality of notes over time.
It's worth remembering that the medical note is not the most important thing that happens during a visit to your doctor. A great note isn’t the same as great care, and vice versa. Still, your medical notes can be a valuable source of health information that differs from all others, including trusted health sites and social media: they’re written by your doctor and they’re all about you.
About the Author
Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. … See Full Bio View all posts by Robert H. Shmerling, MD

Life can be challenging: Build your own resilience plan

Nantucket, a beautiful, 14-mile-long island off the coast of Massachusetts, has a 40-point resiliency plan to help withstand the buffeting seas surrounding it as climate change takes a toll. Perhaps we can all benefit from creating individual resilience plans to help handle the big and small issues that erode our sense of well-being. But what is resilience and how do you cultivate it?
What is resilience?
Resilience is a psychological response that helps you adapt to life’s difficulties and seek a path forward through challenges.
“It’s a flexible mindset that helps you adapt, think critically, and stay focused on your values and what matters most,” says Luana Marques, an associate professor of psychiatry at Harvard Medical School.
While everyone has the ability to be resilient, your capacity for resilience can take a beating over time from chronic stress, perhaps from financial instability or staying in a job you dislike. The longer you’re in that situation, the harder it becomes to cope with it.
Fortunately, it’s possible to cultivate resilience. To do so, it helps to exercise resiliency skills as often as possible, even for minor stressors. Marques recommends the following strategies.
Shift your thoughts
In stressful situations, try to balance out your thoughts by adopting a broader perspective. “This will help you stop using the emotional part of your brain and start using the thinking part of your brain. For example, if you’re asking for a raise and your brain says you won’t get it, think about the things you’ve done in your job that are worthy of a raise. You’ll slow down the emotional response and shift your mindset from anxious to action,” Marques says.
Approach what you want
“When you’re anxious, stressed, or burned out, you tend to avoid things that make you uncomfortable. That can make you feel stuck,” Marques says. “What you need to do is get out of your comfort zone and take a step toward the thing you want, in spite of fear.”
For example: If you’re afraid of giving a presentation, create a PowerPoint and practice it with colleagues. If you’re having conflict at home, don’t walk away from your partner — schedule time to talk about what’s making you upset.
Align actions with your values
“Stress happens when your actions are not aligned with your values — the things that matter most to you or bring you joy. For example, you might feel stressed if you care most about your family but can’t be there for dinner, or care most about your health but drink a lot,” Marques says.
She suggests that you identify your top three values and make sure your daily actions align with them. If being with family is one of the three, make your time with them a priority — perhaps find a way to join them for a daily meal. If you get joy from a clean house, make daily tidying a priority.
Tips for success
Practice the shift, approach, and align strategies throughout the week. “One trick I use is looking at my calendar on Sunday and checking if my actions for the week are aligned with my values. If they aren’t, I try to change things around,” Marques says.
It’s also important to live as healthy a lifestyle as possible, which will help keep your brain functioning at its best.
Healthy lifestyle habits include:
- getting seven to nine hours of sleep per night
- following a healthy diet, such as a Mediterranean-style diet
- aiming for at least 150 minutes of moderate-intensity activities (such as brisk walking) each week — and adding on strength training at least twice a week
- if you drink alcohol, limiting yourself to no more than one drink per day for women and two drinks per day for men
- not smoking
- staying socially connected, whether in person, by phone or video calls, social media, or even text messages.
Need resilience training?
Even the best athletes have coaches, and you might benefit from resilience training.
Consider taking an online course, such as this one developed by Luana Marques. Or maybe turn to a therapist online or in person for help. Look for someone who specializes in cognitive behavioral therapy, which guides you to redirect negative thoughts to positive or productive ones.
Just don’t put off building resilience. Practicing as you face day-to-day stresses will help you learn skills to help navigate when dark clouds roll in and seas get rough.
About the Author

Heidi Godman, Executive Editor, Harvard Health Letter
Heidi Godman is the executive editor of the Harvard Health Letter. Before coming to the Health Letter, she was an award-winning television news anchor and medical reporter for 25 years. Heidi was named a journalism fellow … See Full Bio View all posts by Heidi Godman
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD